Paramedics + Naloxone
In 2007, Brendan Lis entered a stranger’s bedroom. He found an unconscious teenage male in bad shape, wedged between a wall and a bed. He didn’t know it yet, but this was going to be the first time he ever saved a life with Narcan.
| “We went to this house and there was this young kid lying between the bed and the wall and he was snoring. The first thing we did was grab him and put him on our stretcher because there was nothing we could do for him in that position.” – Brendan Lis |
An unconscious patient is a serious challenge, says C.R., a veteran firefighter and paramedic from Peoria, IL, who wanted to remain anonymous. “You are much more on edge when you show up and the person you are trying to help is not awake,” he explains. “You don’t get any of the information you need. You just have to piece it together.”
| “We rushed him out to the truck and did our assessment; in school they teach you all about it. Then we administered it and he was pissed when he woke up. We had to breathe for him on the way to the hospital because he was pretty bad, but the Narcan works really great.” – Brendan Lis |
Most of the time, overdoses are accidental, but not always.
| “Last year when we went to a call on the East Side, a very small person took just enough to overdose on. One shot woke her up. Came up swinging, like they usually do…She overdosed on purpose. She had the pills next to her. We were still checking blood pressure, breathing, oxygen levels, but we gave her the treatment before we finished all of those.” – C.R. |
Heroin and opioid analgesic overdose cases continue to claim thousands of lives on an annual basis. In order to bring light to the issue at hand and to better understand the positive implications of naloxone, we interviewed several paramedics regarding their personal experiences with the drug. Their information is listed near the bottom this article.
The Epidemic
From 2001 to 2013, the National Institute on Drug Abuse (NIDA) recorded a fivefold increase in the number of heroin-related overdose deaths nationwide. The CDC reported a total of 8,257 heroin-related deaths in 2013, in addition to 16,235 prescription opioid analgesic–induced deaths. Furthermore, there were a reported 1,342 fatalities resulting from a combination of heroin and prescription opioids, bringing the total of opioid-induced overdose deaths to a disturbing 25,834.
| “We had found one girl with a needle sticking in her neck. Because the more times you shoot up, the harder it is to find a vein, they sort of retreat into your body. Sort of like a defense mechanism. So someone addicted to heroin is constantly searching for a good vein – so they go from the arms, toes, legs, sometimes the neck – you know you are bad if you are going for the neck. Probably her last vein.” – Brendan Lis |
During the past several years, opioid dependency and heroin-related overdose deaths have become known as a national epidemic. Heroin addicts and those who have become physically dependent on opioid narcotics are not the only ones overdosing – many individuals with no history of substance abuse are falling victim to opiate overdose. Elderly people, post-surgery patients, and nursing home patients have been losing their lives to opiate overdoses, though changes in legal prescription opioid dispensing rules have helped.
In response to the rapidly escalating opioid-related mortality rate, naloxone (a medication used to reverse the effects of overdoses caused by opioids) has become increasingly prevalent within the paramedic community, and it has since saved innumerable lives.
This “wonder drug,” also known as Narcan, has become a key component of many paramedic toolkits nationwide, though availability and distribution still lack throughout some heavily hit areas. Naloxone was distributed in 15 states as of 2010 (the most recent year available), and it’s used frequently in major U.S. cities such as New York City, Baltimore, and Chicago. Potential overdose witnesses (predominantly first-responders) are trained to properly administer the drug in naloxone distribution programs organized by the Department of Health. The antidote can currently be administered intravenously or nasally, although the IV method has proven more rapidly effective.
Naloxone is a potent opioid receptor antagonist. It takes over the receptor cells within the brain, reversing the side effects (and the high) of opioid analgesics and other opiates. This jarring transition leaves the patient stone-cold sober. If they are a long-time user, it may put them in a state of acute opioid withdrawal. The sudden onset of sobriety and withdrawal provides context for the confusion and violence paramedics often see.
Administering naloxone can be dangerous to paramedics as training to deal with violence is not part of their normal curriculum. Patients who have just received a “hit” of naloxone can become aggressive and angry, putting paramedics at risk.
| “When Narcan first came out, they would give them a big enough dose to make sure that they were awake, but then you needed a cop to come with you. Policies changed over time, in part to protect the paramedics.” – C.R. |
Paramedics have since learned which dosages work best to keep patients unconscious while they are being transferred, though the risk of accidental injury persists. While each of the paramedics we interviewed agreed that the benefits of the drug greatly outweigh the potential risks, extensive training needs to be employed alongside any further distribution.
The life-saving potential of naloxone has been helping to avert tragedy in emergency settings since the 1970s – primarily for situations involving heroin overdose. These days, with nearly double the mortality rate, deaths in conjunction with prescription opioid overdose are eclipsing that of heroin. When it comes to heroin and prescription opioid overdoses, the benefits of a pharmaceutical agent like naloxone are hard to dismiss. Placing yourself in situation where overdose is a distinct possibility could be a sign of a larger problem, however. Don’t let opiate or opioid abuse progress to this point – call to speak with someone about your substance rehabilitation options.
Opioids Kill More Than Heroin, So Far …
The term “opioid” refers to a narcotic analgesic that is at least in part synthetic, while the term “opiate” refers to a narcotic analgesic naturally derived from an opium poppy.
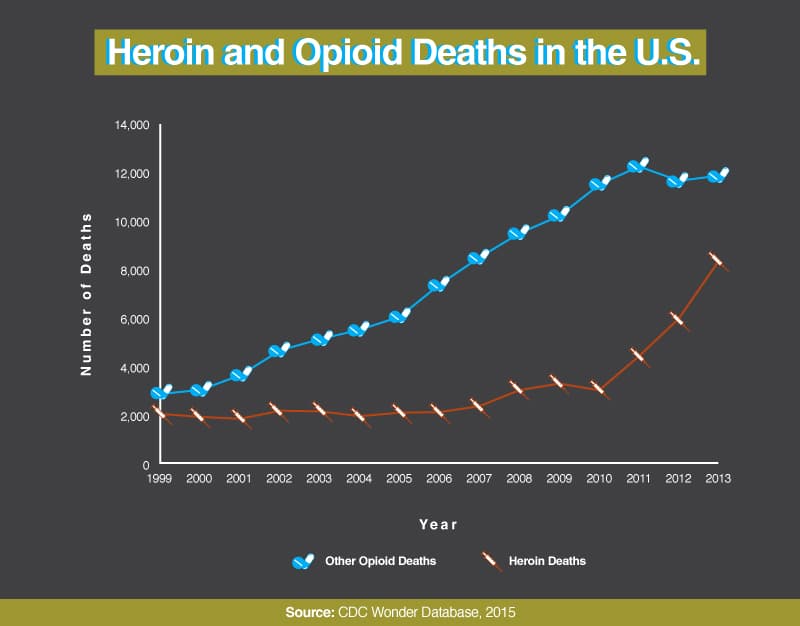
Since 1999, the rates of opioid-related overdose deaths have continued to climb rapidly, increasing more than fivefold in 14 years. While the number of heroin-related fatalities continues to escalate, the number of individuals who are dying at the hands of other opioid narcotics has been increasing at a more severe rate. While nearly 2,000 heroin-related deaths in 1999 has risen to over 8,000 fatalities in 2013, close to 3,000 opioid-related deaths in 1999 skyrocketed to upward of 12,000 in 2011. There were another 12,000 opioid-related deaths in 2013 as well.
It was recently estimated by the CDC that America sees one prescription opioid-related death every 19 minutes. Naloxone is typically associated with heroin overdose, though all interviewed paramedics noted a significant number of prescription opioid overdose cases as well.
| “I’ve seen a lot of teenagers overdosing, but mostly it’s elderly patients. They forgot if they took their medication and take it again and again. Or, sadly, they are in nursing homes, and it is common to keep the patients drugged so they are easier to handle.” – Zabrina Allemang |
| “We usually come across two different kinds of people we give [naloxone] to. First are drug addicts – pill heads, sometimes heroin addicts – and the others are people prescribed some kind of opioid and they accidentally over-medicate – generally old people. We usually find them in bed and the addicts on the floor.” – Brendan Lis |
Prescription opioid overdose has become a major issue among the elderly as well as people suffering from opioid addiction, significantly expanding the potential benefits of widespread naloxone accessibility.
| “Had this one lady – mid 30s – had just had some kind of cosmetic surgery and was prescribed some kind of opiate, and we got a call from her daughter that her mom was in bed and she couldn’t wake her up. When we got there, she was unconscious and she couldn’t be aroused. The first thing we look for when we come across a patient like that is the pupils – when people take take opiates, the pupils can become constricted – that’s the biggest sign – you just look at the pupils and you know.” – Brendan Lis |
What Are the Adverse Effects of Naloxone?
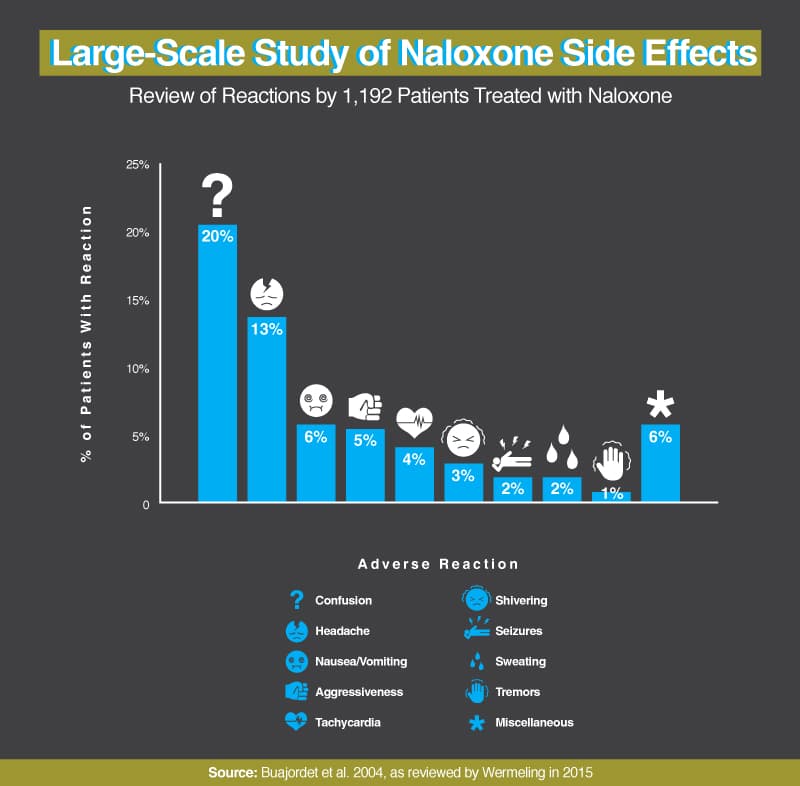
While the adverse side effects of naloxone vary greatly, they generally aren’t severe and subside quickly. In a study of 1,192 patients (all of whom were treated with naloxone and later interviewed), only 6% experienced an adverse reaction that could be considered physically compromising (specifically seizure and tachycardia). Most naloxone patients interviewed (20%) experienced confusion – a seemingly logical side effect considering the circumstances. Headaches were experienced by 13% of interviewed naloxone patients. Other side effects, which were experienced by 17% of interviewed patients in total, include nausea and/or vomiting, aggression, shivering, sweating, and tremors.
Our interviews with paramedics found that they expect about 10% of naloxone patients to wake up violent and problematic.
| “Narcan suppresses the judgment centers in the brain, so sometimes when you give someone a large dose, you are also impairing them mentally. When you’re giving them a big enough dose to knock everything else out, all they see is a bunch of people they don’t know above them – injecting them with stuff, trying to strap them down. And the brain’s suppressed, so all they got is to start swinging.” – C.R. |
| “Sometimes when they wake up they’ll kick, they’ll punch, they’ll bite, they’ll spit, they’ll scratch … They go from high as a kite to stone-cold sober, and very quickly, and so there is something in that transition. When they wake up, they wake up mad.”
“If we give a little too much to the patient, they tend to wake up violent and sometimes they even have projectile vomiting.” – Brendan Lis |
Paramedics told us that when they inject patients with naloxone, they try to provide enough medication to stabilize the patient but not so much that the patient wakes up in a state of aggression. Unless there are extenuating circumstances, leaving patients unconscious until they reach the hospital is the ultimate goal.
| “My mindset is taking care of the patient to the best of my ability. I always try and be careful pushing the Narcan, because I don’t want to end up restraining the patient. I just want them breathing on their own.” – Zabrina Allemang |
Keeping the patient unconscious reduces risk to paramedics, but it does mean walking a fine line. In the past, they gave larger doses of naloxone, paramedic C.R. told us, but these larger doses always woke the patient and made it necessary for a police officer to ride along to handle potential violence. So policy changed.
Overall, the side effects of naloxone are extremely mild compared with the prevalence of fatality when dealing with opioid overdose – the only true risks involve the treating paramedic or first responder, who are the potential target of aggression and violent behavior as the patient is resuscitated.
Who Can Administer Naloxone?
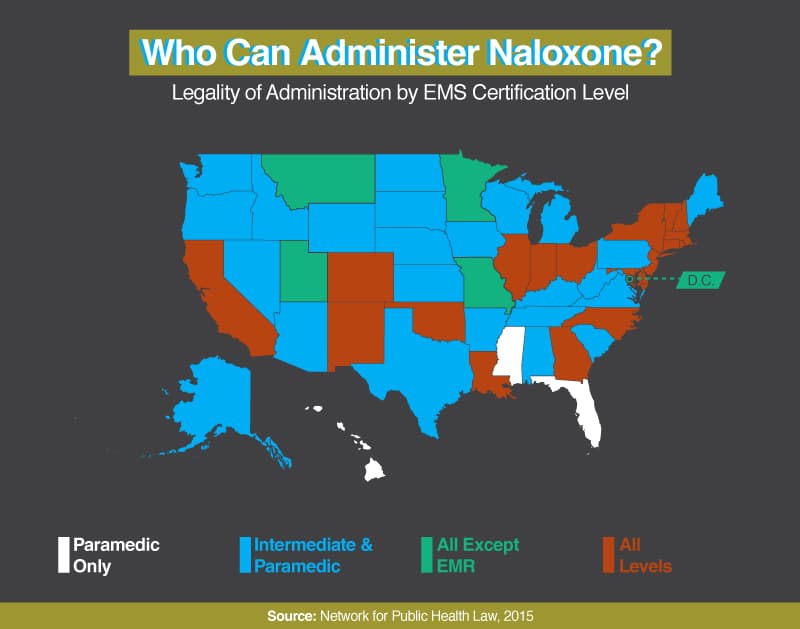
In the United States, naloxone is currently classified as a prescription medication. While it remains legal to prescribe the opioid overdose antidote in every state, the dispensing and distribution of the drug varies significantly by jurisdiction.
Paramedics have legally carried naloxone as a part of their essential “drug box” for years, and while EMS training for naloxone administration was lacking until recently, more paramedics nationwide are being properly trained to administer the drug. Twenty-four states legally allow intermediate EMS (AEMT and EMT-I) and paramedics to carry and administer naloxone. Five states allow all levels of EMS aside from EMR to carry and administer naloxone, and 19 states allow all levels of first responders to carry and dispense the drug. Only three states – Hawaii, Florida, and Mississippi – allow paramedics exclusively to administer the drug.
| “There is talk about here, in Illinois, that Narcan is going to become an OTC medication. On the one hand I’m happy because you can get some people, the elderly, who are forgetful and don’t know, they might not realize how many doses they took, and if they had a few of those on hand, a relative could give it to them. Just a pill – here you go.” – C.R. |
| “If a completely inexperienced person gave naloxone to somebody, it wouldn’t be doing any harm to them, really.” – Brendan Lis |
While many medical personnel are pushing for nationwide legalization, there are still potential issues regarding widespread distribution. Some political figures believe that making naloxone available to a greater variety of first responders and to the general public will adversely enable drug users. This concern, though not yet backed with any substantial scientific evidence, leads states such as Florida to permit only paramedics to administer the drug (despite a dramatic increase in opioid-related deaths over the past several years). It is also essential that other first responders, as well as members of the general public with access to naloxone, learn to properly administer the drug if accessibility continues to expand. While naloxone has been proven to obstruct overdose-induced fatality, patients may still need professional medical attention.
While barriers exist, both legally and politically, they haven’t stopped untrained citizens from administering naloxone. The CDC reports that non-professionals (members of the general public) reversed 26,463 overdoses with naloxone between 1996 and June 2014.
Naloxone, while having undisputed benefits, is no failsafe countermeasure to every overdose situation. Don’t place yourself in harm’s way in the first place. If you or someone close to you are struggling under the weight of heroin or prescription painkiller abuse, call now. Speak confidentially with a caring treatment support specialist about substance abuse treatment programs that can help.
Who Buys Naloxone?
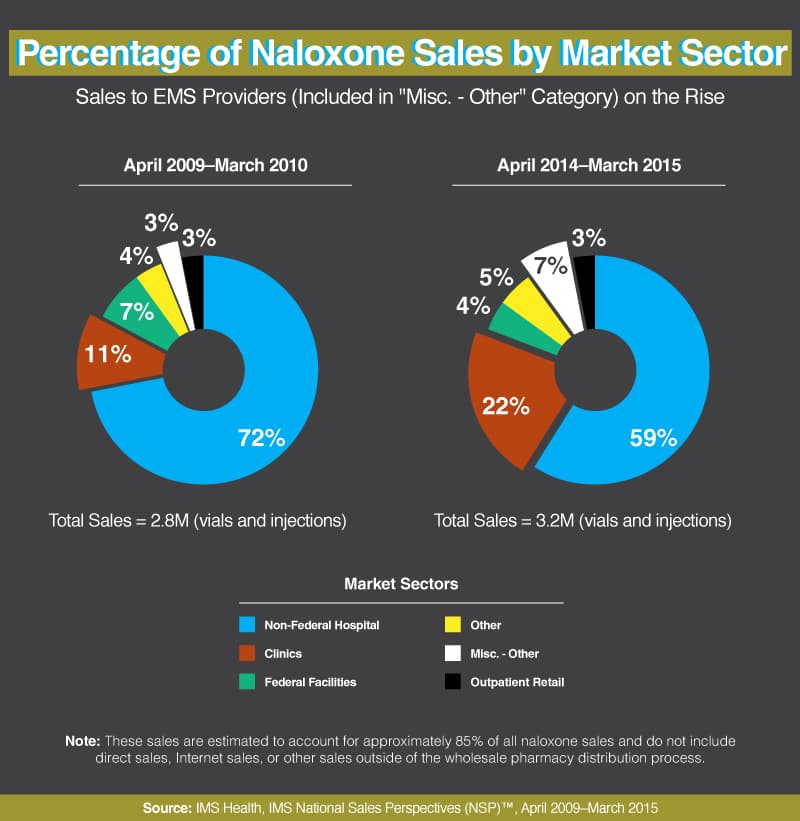
Naloxone sales to paramedic organizations and medical clinics – both outpatient settings – have increased significantly in the past five years, with distribution to clinics more than doubling in size. Meanwhile, sales to hospitals have shrunk as the market has grown.
This growth seems logical, considering the great enthusiasm with which all of the interviewed paramedics discussed the drug. “I think it is a great creation and will be very helpful in giving some people a second chance at life,” Boynton Beach, FL, paramedic John Marisola noted. Brendan Lis, another Florida paramedic, explained that naloxone is his “favorite drug in [the] drug box.”
Increasing popularity of the drug among emergency medical technicians is a direct result of its increased need. As more men and women fall victim to opioid overdose, more lives are congruently being saved by the drug – and more clinics and paramedics are incorporating naloxone into their kit of essentials.
New Products and Competition,
but Prices Still Skyrocket
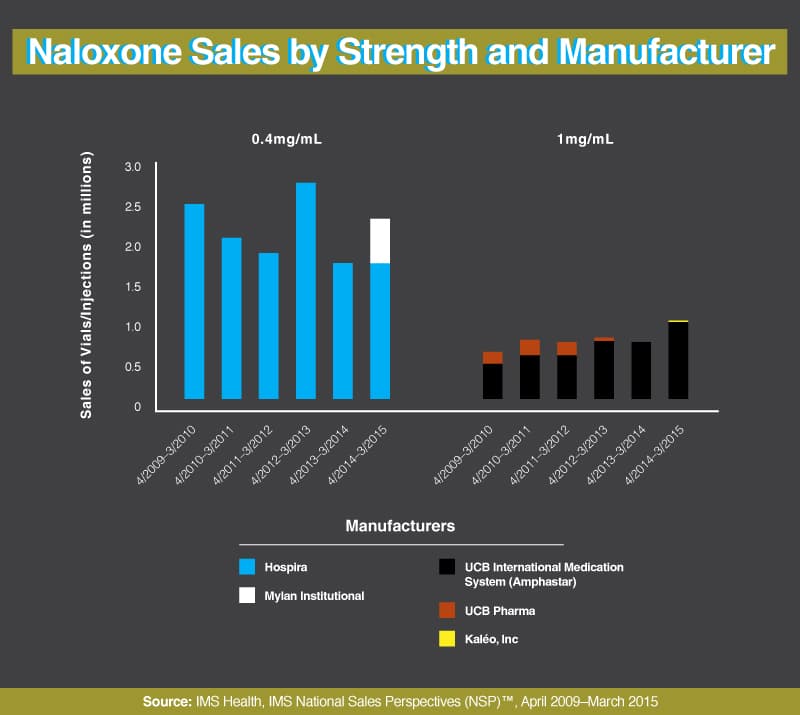
The majority of paramedics and other naloxone-equipped first responders use 0.4 mg of naloxone, manufactured by Hospira. From April 2014 to March 2015, a new brand of 0.4 mg intravenous shot has come to be used prevalently as well – one manufactured by the Mylan Institutions.
A plethora of new products have been entering the market since 2009. Naloxone distributed by name brands such as UCB International Medications Systems (Amphastar), UCB Pharma, and Kaléo Inc.? has become available as competition increases. These three companies produce a higher dosage version, all manufacturing products that contain 1 mg as opposed to 0.4 mg (though the standard 0.4 mg products remain the most popular amongst paramedics). Higher-dose products are often used in alternative delivery systems, like those designed for nasal application, which has a lower absorption rate.
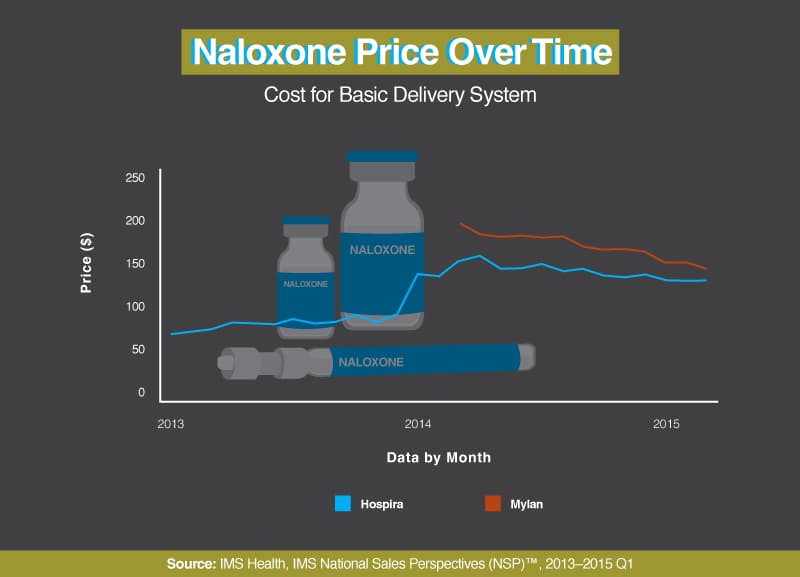
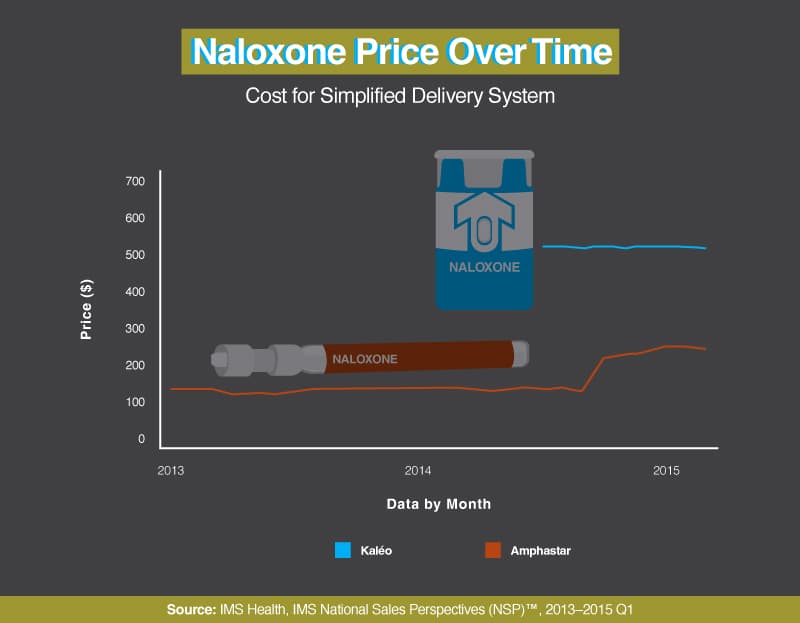
Naloxone manufactured by Mylan is significantly more expensive than that manufactured by Hospira, though the cost of Hospira-made naloxone has been steadily increasing while the naloxone manufactured by Mylan has been gradually declining in cost over the past year. In January 2014, the cost of Hospira’s product increased by 50%. Naloxone manufactured by Kaléo was first introduced in July 2014 and was initially priced at roughly four times as much as the Amphastar product. Kaléo pricing has remained consistent, while the cost of Amphastar increased nearly 60% in September 2014.
While price increases of naloxone are a political issue, the cost of EMS is not affected.
| “The price of Narcan will not change whether or not we carry it – it is worth losing money to save a life. And Narcan is still relatively cheap considering other supply costs.” – Zabrina Allemang |
Despite increasing costs and competition, Hospira remains the most affordable and widely used brand of naloxone – and is the brand predominantly used by paramedics and all other emergency medical technicians nationwide.
Conclusion
Narcan is the primary weapon paramedics use in the war against opioid-related overdoses. Even with their heroic efforts, 43,982 men and women lost their lives to opioid overdoses in 2013 alone.
A first responder’s job is done when they drop a patient off at the hospital; they never really know what happens after that. They saved a life, at least temporarily, but did that person survive and prosper? Did they get into treatment and find a better life?
The truth is that many do not. Even being brought back to life with naloxone is not a wakeup call for everyone; the addiction is that strong. According to Dr. Edward Bernstein, 30% of those revived at Boston Medical Center have been revived more than once.
If you or someone you love is battling a substance abuse disorder, especially one involving prescription opioids or heroin, seek help. Don’t wait for an overdose or near-overdose to proactively seek treatment. Reach out to our caring treatment support team of Rehabs.com at today for rehabilitation guidance.
Interviewees
|
|
Fair Use Statement
Please feel free to share the images and information found on this page. When doing so, we ask that you kindly attribute the creators of this project by providing your readers with a link back to this page so they can read more about the research and our methodology.